Ask a physician if Radixact treatment is right for you
You deserve the best possible treatment for your brain tumor. Find a physician in your area offering the Radixact System – and find out if Radixact treatment is right for you.
Brain tumors can affect different senses and/or memory depending on their location. That’s why when it comes to treating the complex, delicate and vital tissues and structures of the brain, precision matters.
Advances in care mean there are better options for people diagnosed with brain tumors, helping to ensure they receive the most effective treatment for their particular medical condition. Radiation therapy may be one treatment option and can be used to treat the two main types of brain tumors:
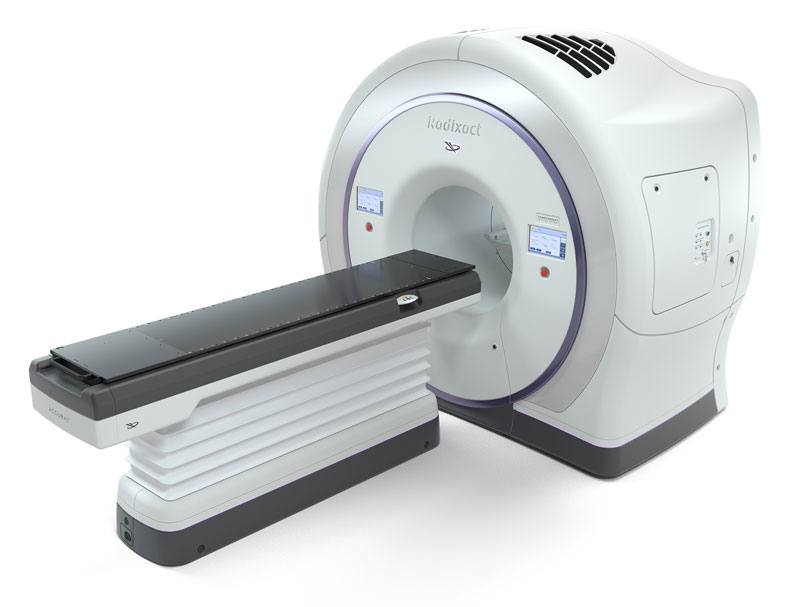
Radiation therapy is a proven treatment for brain tumors and is either used after surgery to kill any remaining tumors cells, or as the main treatment option when surgery is not an option. The Radixact System, featuring TomoTherapy technology, combines multiple 360-degree treatment delivery with powerful dose-sculpting capabilities, providing greater control of the radiation dose so it conforms precisely to the tumor and minimizes damage to healthy tissue(s). The result is a radiation therapy treatment that maximizes effectiveness, while helping to preserve important brain or cognitive functions like memory and minimize the risk of potential side effects that can impact short- and long-term quality of life.
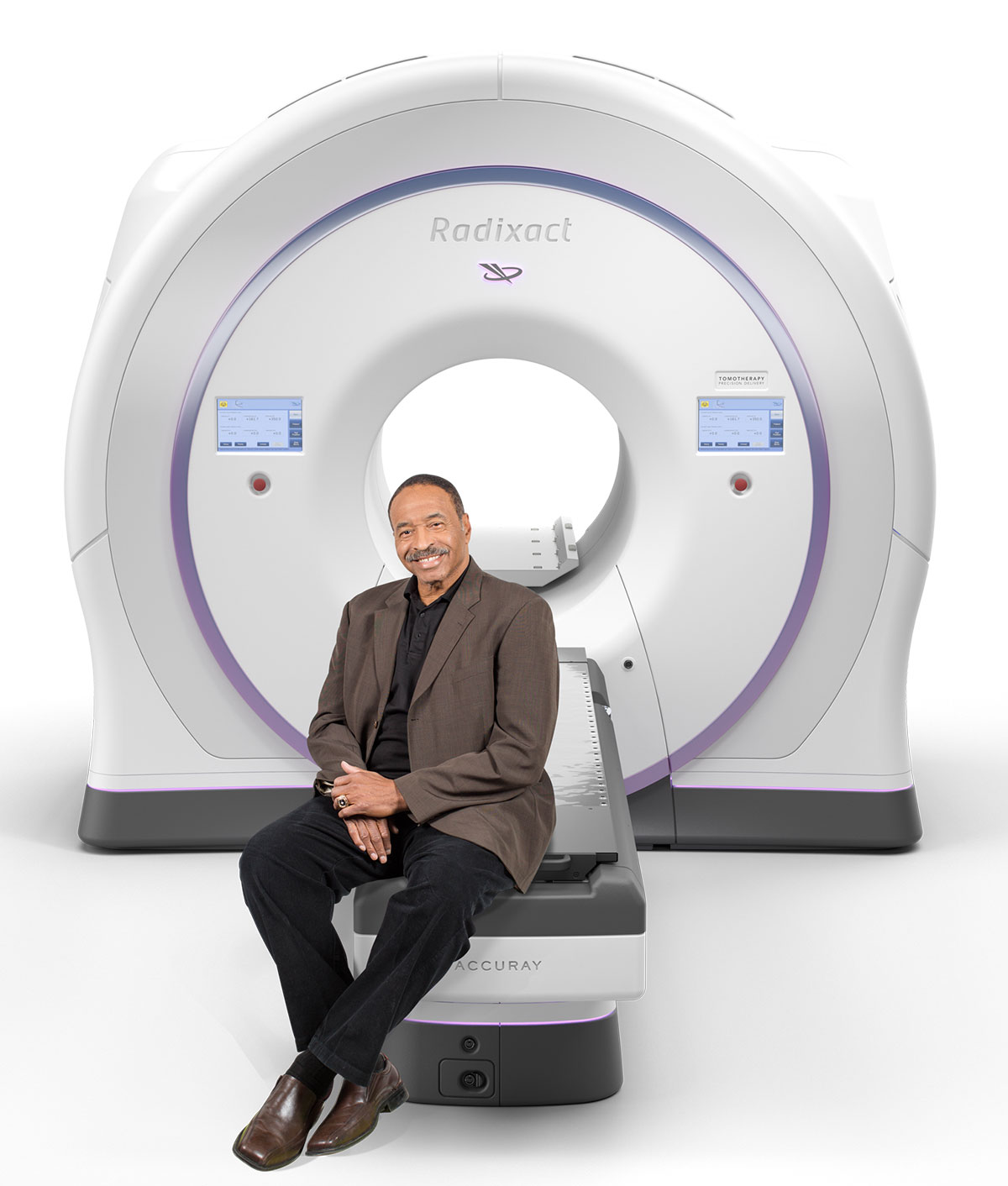
You deserve the best possible treatment for your brain tumor. Find a physician in your area offering the Radixact System – and find out if Radixact treatment is right for you.
Clinically Proven Outcomes
A Non-Invasive Option
Radixact vs. Traditional Treatments
Enabling Re-treatment
The Radixact System, the next-generation TomoTherapy platform, is one of the most integrated, advanced systems for comprehensive cancer treatment available today. The Radixact System enables precise delivery of radiation for the treatment of single and multiple brain tumors. The TomoTherapy technology is supported by published clinical studies, and has been proven to reduce the dose delivered to surrounding tissues.

Clinical research supports the use of the TomoTherapy technology used in the Radixact System for the treatment of brain tumors. Listed below are key studies to support your discussion of Radixact with your doctor.
The precision of surgical intervention may improve outcomes for many brain tumors, but there are many cases where surgical intervention may not be possible – or simply may not be the best option available. Radiation therapy is proven to provide a non-surgical, non-invasive treatment option for many brain tumors. Your doctor may use radiation therapy after surgery to try to kill any remaining tumor cells as the main treatment if surgery is not a good option and medications are not effective, or to help prevent or relieve symptoms from the tumor.
The Radixact System offers a non-surgical, non-invasive option that is proven effective in treating a broad spectrum of brain tumors of all stages and complexities, and brain metastases. The Radixact System is also a proven option for delivering craniospinal irradiation for patients with central nervous system malignancies, such as medulloblastoma and primitive neuroectodermal tumors.
The Radixact System provides the flexibility to adapt radiation therapy to any patient’s brain cancer anatomy, helping to enable the delivery of extremely precise and accurate radiation doses to improve treatment outcomes and help reduce the risk of side effects that may impact patients’ quality of life.
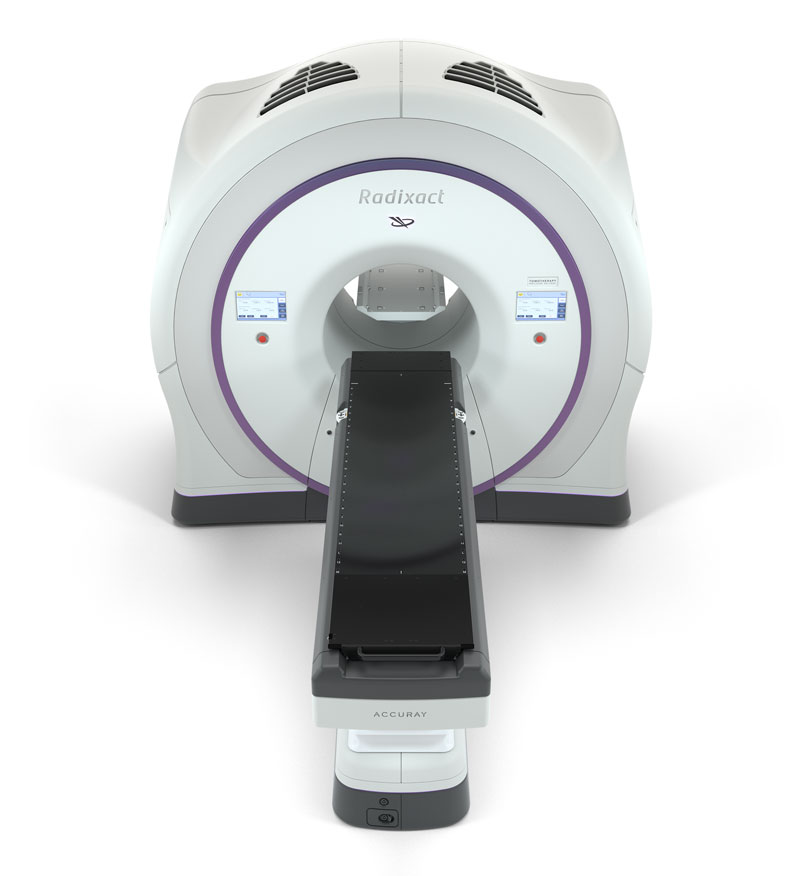
The Radixact System with TomoTherapy technology maximizes radiation delivered to the target — while helping to minimize dose to surrounding healthy tissues. The result is highly personalized treatment designed to significantly reduce the risk of the side effects that too often disrupt the lives of patients during and after treatment.
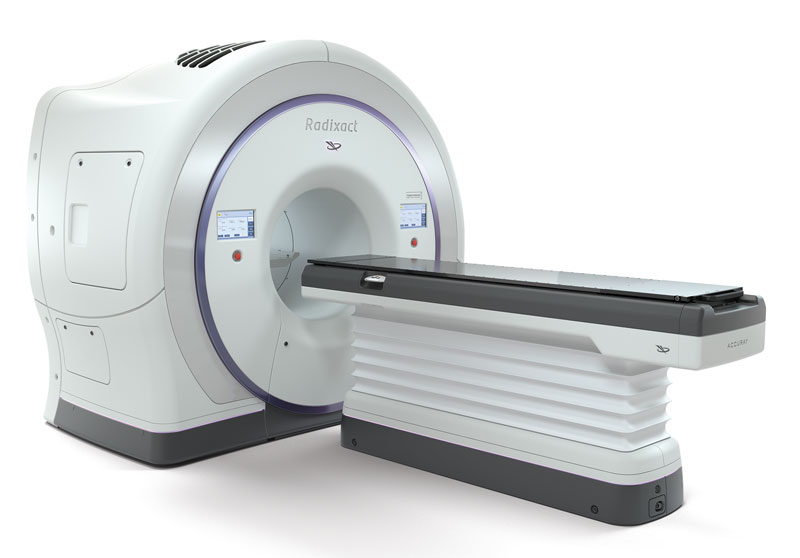
Image-guided intensity-modulated radiation therapy (IG-IMRT) with the Radixact System, the next-generation TomoTherapy platform, can offer an effective alternative in many cases, delivering precision in a non-invasive, outpatient procedure that does not require incisions or general anesthesia. Most patients will not require hospitalization or a long recovery period.
Radixact treatment is an outpatient procedure that does not require incisions or general anesthesia. Most patients will not require hospitalization or a long recovery period.
Because the precise targeting of the Radixact System significantly reduces irradiation of surrounding healthy tissues, the Radixact System can be a powerful treatment option for patients with brain tumors, including patients who have previously undergone radiation or surgical procedures, and experience a recurrence.
References:
1 Bruni A, Gaito S, Ciarmatori A, et al. Radiosurgery Using Tomotherapy for Patients with Brain Oligo-metastasis: A Retrospective Analysis on Feasibility and Tolerance. Anticancer Res. 2015 Dec;35(12):6805-12. PMID: 26637900.
2 Barra S, Agostinelli S, Vagge S, et al.Radiosurgery with Helical Tomotherapy: Outcomes for Patients with One or Multifocal Brain Metastasis. Technol Cancer Res Treat. 2015 Dec;14(6):693-9.
3 Koide Y, Tomita N, Adachi S, et al. Retrospective analysis of hypofractionated stereotactic radiotherapy for tumors larger than 2 cm. Nagoya J Med Sci. 2019 Aug;81(3):397-406.
4 Nagai A, Shibamoto Y, Yoshida M, et al. Treatment of single or multiple brain metastases by hypofractionated stereotactic radiotherapy using helical tomotherapy. Int J Mol Sci. 2014 Apr 22;15(4):6910-24.
5 Boulle G, Bracci S, Hitchcock K, et al. Treatment of grade II-III intracranial meningioma with helical tomotherapy. J Clin Neurosci. 2019 Jan;59:190-196.
6 Donato V, Caruso C, Bressi C, et al. Evaluation of helical tomotherapy in the treatment of high-grade gliomas near critical structures. Tumori. 2012 Sep-Oct;98(5):636-42.
7 Sun Y, Liu G, Chen W, et al. Dosimetric comparisons of craniospinal axis irradiation using helical tomotherapy, volume-modulated arc therapy and intensity-modulated radiotherapy for medulloblastoma. Transl. Cancer Res. 2019;8.
8 Sugie C, Shibamoto Y, Ayakawa S, et al. Craniospinal Irradiation Using Helical Tomotherapy: Evaluation of Acute Toxicity and Dose Distribution. Technol. Cancer Res. Treat. 2011;10:187–195.
9 Mesbah L, Matute R, Usychkin S, et al. Helical tomotherapy in the treatment of pediatric malignancies: a preliminary report of feasibility and acute toxicity. Radiat. Oncol. 2011;6:102.
10 Koca T, Basaran H, Sezen D, Karaca S, Ors Y, Arslan D, Aydin A. Comparison of linear accelerator and helical tomotherapy plans for glioblastoma multiforme patients. Asian Pac J Cancer Prev. 2014;15(18):7811-
11 Chan M, Schupak K, Burman C, Chui C, Clifton Ling C. Comparison of intensity-modulated radiotherapy with three-dimensional conformal radiation therapy planning for glioblastoma multiforme. Medical Dosimetry. 28(4);261-5