Ask a physician if Radixact treatment is right for you
You deserve the best possible treatment for your breast cancer. Find a physician in your area offering the Radixact System — and find out if Radixact treatment is right for you.
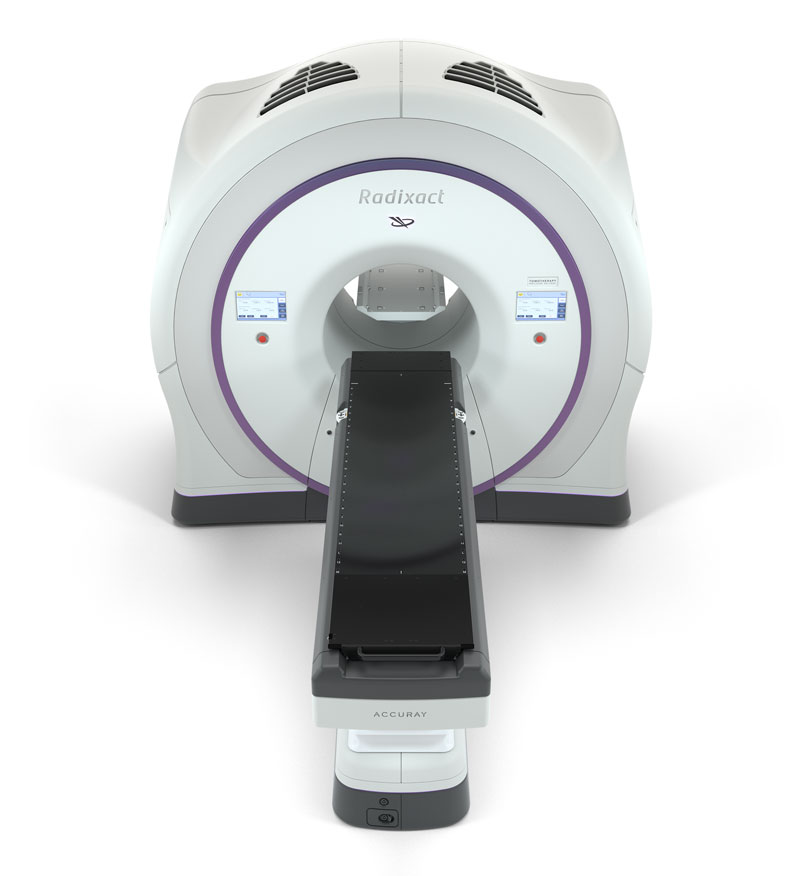
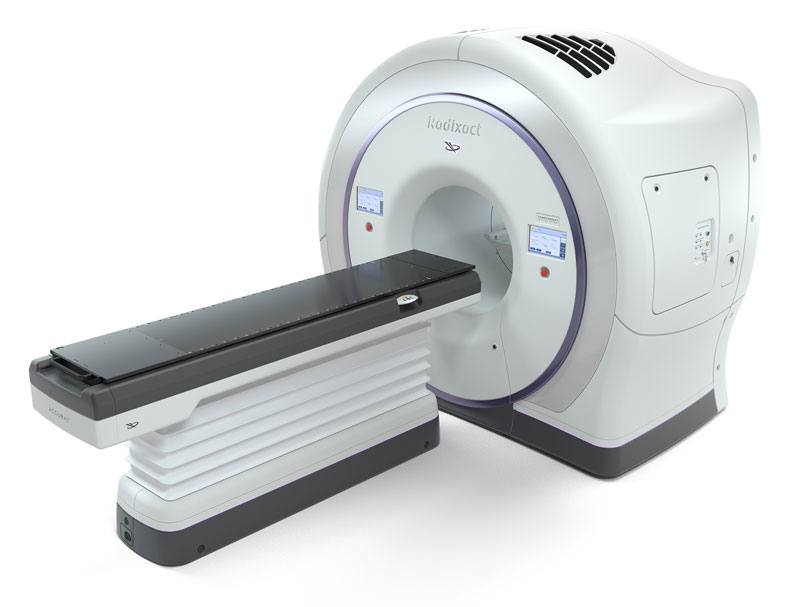
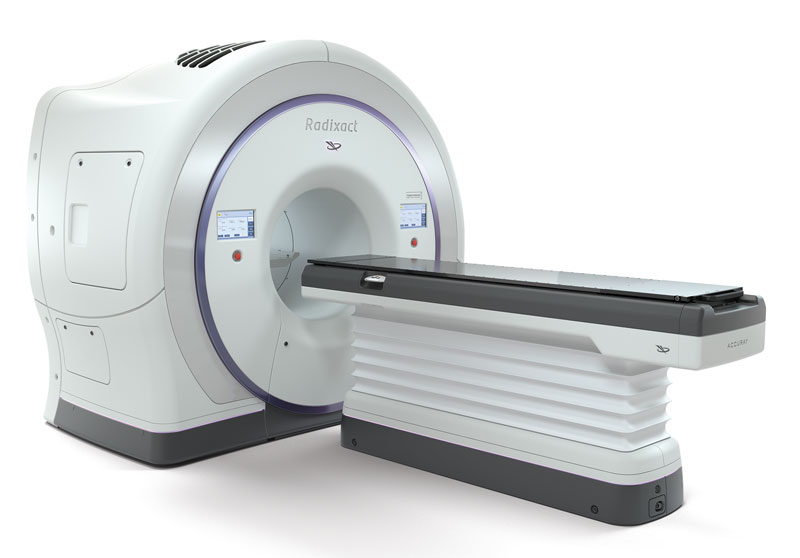
You have more options than ever for effectively treating breast cancer. But there is no one-size-fits-all treatment. You are unique. Your body, your lifestyle, your values and the specifics of your cancer all play a role in shaping your ideal treatment. The Radixact® System provides a personalized, precise and non-invasive option for treating your breast cancer, typically post lumpectomy or mastectomy. The system is the world’s only helical radiotherapy platform, delivering highly accurate radiation dose from 360 degrees around the patient.
The Radixact System with the TomoTherapy® technology is designed to help improve clinical outcomes, while minimizing the risk of side effects, to protect your quality of life both during and after treatment. Two treatment delivery modes (TomoHelical™ and TomoDirect™) offer unique advantages in the treatment of breast cancer, including the ability to deliver precise radiation dose to any tumor or tumor bed, during every treatment, while minimizing dose to nearby healthy organs and tissues. This is especially important for women diagnosed with cancer in the left breast, where the tumor may be close to critical organs such as the heart.

You deserve the best possible treatment for your breast cancer. Find a physician in your area offering the Radixact System — and find out if Radixact treatment is right for you.
The Radixact System with TomoTherapy technology is one of the most integrated, advanced systems for comprehensive cancer treatment available today and can be used to treat the full spectrum of breast cancers — from routine to complex tumors, those located in hard-to-reach areas and recurrent tumors. Several studies conducted using the TomoTherapy technology have shown good results.

Radiation therapy may be used to treat breast cancer at almost every stage and can be used after surgery, chemotherapy and other medications. It is commonly used to help reduce risk of breast cancer recurrence and also can be used to provide relief from symptoms, such as pain, associated with advanced breast cancer.
The Radixact System provides the flexibility to adapt radiation therapy to any breast cancer patient’s anatomy, maximizing the radiation delivered to cancerous tissue while minimizing dose to the heart, lungs, other sensitive organs and surrounding healthy tissue.
Treatment with the system is a non-surgical, non-invasive, outpatient procedure that does not require incisions or general anesthesia. Most patients will not require hospitalization or a long recovery time.
Because the precise targeting of the Radixact System significantly reduces irradiation of surrounding healthy tissues, breast cancer patients treated with the Radixact System may sometimes be candidates for surgical interventions, in the event of recurrence. Under certain circumstances, patients may also undergo additional radiation treatments.
The Radixact System maximizes radiation delivered to the target — while helping to minimize dose to surrounding healthy tissues. The result is highly personalized treatment designed to significantly reduce the risk of the side effects that too often disrupt the lives of patients during and after treatment. Studies support the use of the TomoTherapy System for the treatment of breast cancer and show evidence of very good tumor control2, 6, 7, 8 with minimal radiation delivered to surrounding organs at risk (heart, lungs, etc.) and healthy tissues, and low toxicity3,4. The treatment regimens described in the studies reinforce the benefits of the unique capabilities of the TomoTherapy platform and what clinicians and their patients could expect to see with the Radixact System.
Radixact treatment is an outpatient procedure that does not require incisions or general anesthesia. Most patients will not require hospitalization or a long recovery period.
Radixact treatment eliminates the inconvenience and risk associated with radioactive seed or catheter implants.
References:
1 Buwenge M, Cammelli S, Ammendolia I, et al. “Intensity modulated radiation therapy for breast cancer: current perspectives.” Breast Cancer Targets Ther. 2017;9:121–126.
2 Franco et al. “Intensity-modulated and hypofractionated simultaneous integrated boost adjuvant breast radiation employing statics ports of TomoTherapy (TomoDirect): a prospective phase II trial.” J Cancer Res Clin Oncol. 2014 Jan;140(1):167-77. doi: 10.1007/s00432-013-1560-8.
3 Caudrelier et al. “IMRT sparing of normal tissues in locoregional treatment of breast cancer.” Radiat Oncol. 2014 Jul 22;9:161. doi: 10.1186/1748-717X-9-161.
4 Chitapanarux I, Nobnop W, Tippanya D et al. “Clinical outcomes and dosimetric study of hypofractionated Helical tomotherapy in breast cancer patients.” PLoS One. 2019 Jan 31;14(1):e0211578.
5 Arsene-Henry A, Foy JP, Robilliard M et al. “The use of helical tomotherapy in the treatment of early stage breast cancer: indications, tolerance, efficacy-a single center experience.” Oncotarget. 2018 May 4;9(34):23608-23619.
6 O’Donnell et al. “Early Experience of TomoTherapy-based Intensity-modulated Radiotherapy for Breast Cancer Treatment.” Clinical Oncology 2009 21: 294-301.
7 Van Prijs et al. “Short course radiotherapy with simultaneous integrated boost for stage I-II breast cancer, early toxicities of a randomized clinical trial.” Radiation Oncology 2012, 7:80.
8 Michalski et al. “A dosimetric comparison of 3D-CRT, IMRT and static tomotherapy with an SIB for large and small breast volumes.” Medical Dosimetry. 2014 Summer;39(2):163-8. doi: 10.1016/j.meddos.2013.12.003.
© 2024 Accuray Incorporated. All rights reserved.
Educating others about your experience with the Radixact® or TomoTherapy® System can help others who face similar decisions about their own cancer treatment choices.
If you are interested in sharing your story, please fill out the form below and an Accuray representative will contact you.