TREATMENT
Approximately one to two weeks after your treatment plan is finalized, you will begin treatment sessions. Treatment sessions are non-invasive outpatient procedures, and nothing will be required of you during treatment. No patient restraints. No anesthesia.
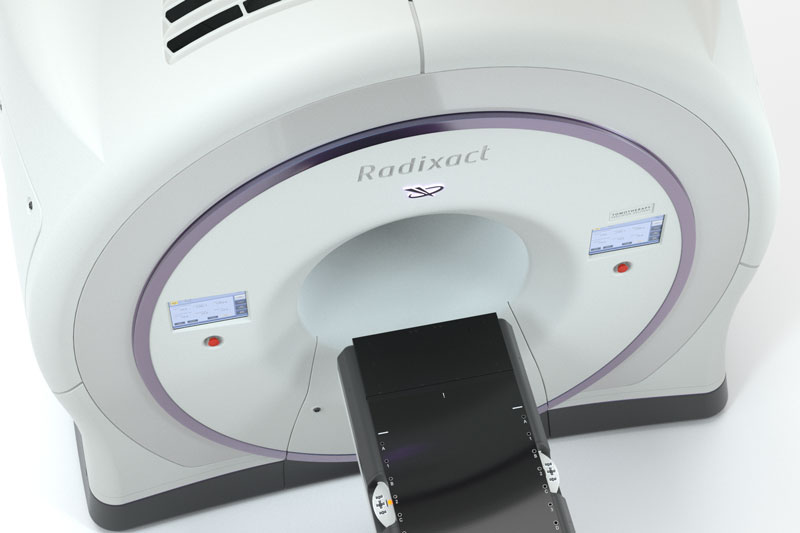
On each treatment day, you will be carefully positioned on the treatment couch. The Radixact System acts as both a CT scanner and treatment delivery machine. This unique combination enables doctors to take a CT scan immediately before each treatment. With that image, they can verify the position of the tumor and, if necessary, adjust your position to help make sure radiation is delivered with high precision.
Once the short imaging procedure is complete, treatment delivery will begin. As the Radixact patient couch moves you at a deliberate pace through the center of the gantry, radiation beamlets are delivered precisely to the treatment area from 360 degrees. If the Synchrony® technology* is used to synchronize and adapt the beams to your breathing and tumor motion, you will undergo a short procedure between imaging and treatment delivery to create a breathing model that will help predict your breathing cycle.
You can expect your Radixact treatment to require daily sessions for 6-8 weeks. Because the Radixact System can deliver radiation continuously, without requiring interruptions to reposition, the entire treatment process typically lasts 10-20 minutes — including patient set-up time.